Sterilization methods are crucial in keeping hospitals and other medical facilities germ-free, helping prevent infections and the spread of diseases. While steam and ethylene oxide gas (EOG) approaches have been around for many years, vaporized hydrogen peroxide (VHP) sterilization is a newer method that outperforms these traditional techniques in many ways.
If you are considering using VHP in your facility, this guide will teach you everything that you need to know.
What Is Vaporized Hydrogen Peroxide Sterilization?
VHP sterilization is a low-temperature sterilization technique for heat-sensitive medical devices and instruments. Low-temperature processes use gas or other chemicals for items that may be damaged by steam. Though EOG used to be the main sterilant in this process, VHP is becoming increasingly popular.
The VHP method involves vaporizing hydrogen peroxide to blast it into an enclosure, creating a sterile solution that effectively removes viruses, spores, mycobacteria, bacteria and fungi from medical equipment. Afterward, the process is reversed, breaking down the hydrogen peroxide into water and oxygen to avoid safety risks linked to the residue of this substance. Some hydrogen peroxide sterilizers also use ozone or plasma to help remove this residue.
Why Use Vaporized Hydrogen Peroxide For Sterilization?
The VHP sterilization process offers many benefits, including the ability to kill microorganisms without high heat. Compared to other methods, using hydrogen peroxide may be quicker, safer, and more energy-efficient.
Using hydrogen peroxide for sterilization has the following advantages:
- Enhanced safety: While EOG also doesn’t rely on heat, this method has significant health and safety concerns. This gas is toxic, and exposure can cause various symptoms ranging from dizziness to difficulty breathing. Due to this toxicity, aeration is necessary after sterilization to remove dangerous residues from instruments and minimize the risk of exposure. VHP and its residues of water and vapor are non-toxic, making it a much safer option with shorter aeration times.
- Faster cycles: VHP can complete the sterilization process in under an hour, supporting greater time efficiency than EOG and steam methods. Steam sterilization involves much longer cycles, whereas EOG processes require several hours of ventilation. With its quick cycle, VHP can help increase your facility’s workflow.
- Reduced energy consumption: VHP sterilization operates at a lower temperature and uses much less energy than steam sterilization, which requires extensive water evaporation.
- FDA approved: The U.S. Food and Drug Administration (FDA) announced that it considers VHP an established method of sterilization for medical devices and recognized its extensive history of safety and effectiveness in 2024. This announcement forms part of the agency’s plan to encourage the wider adoption of VHP as a sterilant and reduce the use of EOG.
What Can You Sterilize With Vaporized Hydrogen Peroxide?
Materials and medical items that can’t tolerate heat and humidity can be sterilized with VHP. For example, endoscopes are made from polymeric components, which shouldn’t be exposed to temperatures above 140 degrees Fahrenheit. As steam sterilization involves temperatures as high as 250 degrees Fahrenheit, this method would likely damage endoscopes and other surgical devices with delicate parts. As the hydrogen peroxide sterilization process’s temperature range is between approximately 98 and 111 degrees Fahrenheit, it is much more suitable.
Additional heat-sensitive instruments, devices and materials that can be sterilized with VHP include:
- Certain types of plastics, such as polypropylene and polyethylene.
- Electrical devices.
- Metal alloys that are susceptible to corrosion, such as brass.
- Medical implants.
How to Sterilize With Vaporized Hydrogen Peroxide
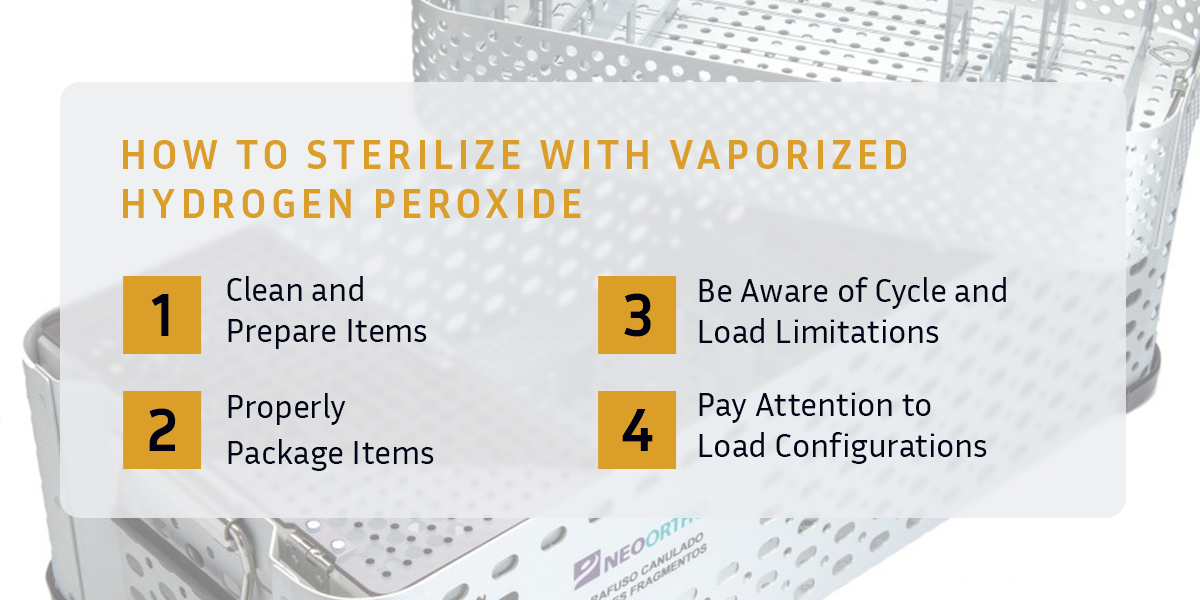
Though VHP is a highly effective sterilant and plays a vital role in health care, the tasks performed before sterilization also have an impact on the success of this process. There is no room for error — improper sterilization can be fatal. Hospital workers must follow the necessary procedures and protocols to help reduce the likelihood of infection and other safety hazards.
By following these steps, you or your workers can help ensure successful sterilization with VHP.
1. Clean and Prepare Items
You must thoroughly clean and dry devices and instruments before they undergo sterilization.
If items have any residual blood or protein left on them, the VHP may be used to remove this excess residue rather than kill microbes. Additionally, large amounts of trapped moisture may cause complications with the sterilizer machine, causing it to pause its cycle. Even smaller amounts of water can be problematic.
For example, droplets inside an endoscope’s lumen can freeze once exposed to the machine’s vacuum, creating a blockage and hindering the VHP’s penetration. In this case, any bacteria would be shielded from the salient.
Cleaning and drying items beforehand can make it easier for the hydrogen peroxide to fulfill its critical function.
2. Properly Package Items
Once you or your workers have inspected the items to verify that they are clean and completely dry, package them into a containment device, such as peel pouches and packs, sterilization trays or sterilization container systems.
No matter what you use, ensure you purchase your containers from a reputable manufacturer, such as Jewel Precision, that offers quality and durability. With a dependable supplier, you will have peace of mind that your devices are protected and secure.
When packing devices or instruments, evenly distribute them in the containment device. Doing so can allow the VHP to contact every inch of the item’s surface. If you need to disassemble something before you can pack it, always refer to the manufacturer’s usage instructions.
You should also ensure that all items are at the correct temperature before being sterilized — devices or instruments that are too cold can result in the condensation of VHP. Though it can be rare, this moisture may cause the same issues as inadequate drying of items. To err on the side of caution, do not place items directly beneath an air conditioner before they are sterilized.
3. Be Aware of Cycle and Load Limitations
Many VHP sterilizer machines have cycle and load limitations, including:
- Whether different types of devices can be processed together in a cycle.
- The number of devices that can be sterilized simultaneously.
- How much weight the sterilizer can handle.
Processing too many items in a cycle or overloading the machine can restrict the sterilizer’s effectiveness.
Awareness of your machine’s limitations is essential for proper sterilization, so always refer to the usage manual and adhere to the manufacturer’s recommendations.
4. Pay Attention to Load Configurations
When placing containment devices into the sterilizer’s chamber, ensure that they are flat and in the center of the shelf unless otherwise specified by the sterilizer or containment device manufacturer.
VHP sterilizers that use plasma typically feature a coil inside the chamber, which can limit the available space. Be cautious of letting containment devices touch this coil, which may disrupt the cycle.
Potential Challenges of Sterilizing With Vaporized Hydrogen Peroxide
Even though VHP has many benefits, you may face some key challenges when using this sterilant. You can determine whether hydrogen peroxide is the right choice by balancing the advantages and possible drawbacks.
Some of the disadvantages of sterilizing with VHP may include:
- Small chambers: The chambers of hydrogen peroxide sterilizers are generally smaller than steam sterilizers or autoclaves, explaining the cycle and load limitations. With the volume of your batches restricted, sterilizing with VHP may take longer as it can require additional cycles.
- Extensive protocol: The pre-processing required before devices or instruments are sterilized can be time-consuming.
- Material limitations: Some materials are not suited to this method because they are sensitive to moisture or oxidants. For example, you shouldn’t sterilize powders, linens, cellulose materials and liquids with VHP.
Choosing the correct sterilization method is a matter of selecting what is best for the instruments and equipment. If you need to process heat-sensitive items, VHP can work. However, steam sterilization in an autoclave is likely a wiser choice, as you will likely enjoy a machine with a greater chamber and a larger load capacity without worrying about hydrogen peroxide exposure.
Sterilize Your Medical Equipment With Jewel Precision
Jewel Precision manufactures custom sterilization cases for medical equipment that we can tailor to your facility’s specifications.
As an industry leader since 1984, we have spent decades perfecting our case-making process. We also use only the most durable materials and advanced designs to create products that health care workers and other medical professionals can trust.
To learn more about our products or request a free quote, contact us today!
