
{
“@context”: “https://schema.org/”,
“@type”: “HowTo”,
“name”: “How to Reduce Hospital Acquired Infections in the OR”,
“description”: “The first step toward reducing HAIs in any health care facility starts with creating a plan for identifying and addressing the most common pathogens in your facility. You must make sure everyone knows the best practices for preventing infection spread and follows through with them every time they care for patients.”,
“step”: [{
“@type”: “HowToStep”,
“text”: “On the team should be at least one expert in diseases and their spread. This professional can help team members identify means of pathogen transmission in ORs and other parts of the hospital and how to prevent them. The infectious diseases expert should also serve as a consultant for renovations or construction projects to ensure the facility has a protective design against disease spread.”,
“name”: “Create an Antimicrobial Control Team”
},{
“@type”: “HowToStep”,
“text”: “Identify the pathogens that have affected patients in your facility infected with HAIs. By knowing the specific diseases causing infections, physicians can avoid unnecessarily prescribing antibiotics. Additionally, train staff on the pathogens that appear most often in your facility and other potential infection sources. Staff members should know what they’ll face and how the diseases spread. Some bacteria are airborne while others spread through surface contact or blood contamination.”,
“name”: “Identify Problem Pathogens”
},{
“@type”: “HowToStep”,
“text”: “Any instruments or equipment that come into direct contact with body fluids or sterile body tissues fall under the category of critical items. Properly done, sterilization kills all microorganisms on the surfaces of medical instruments. On the other hand, improperly sterilized equipment raises the risk of pathogen transmission.”,
“name”: “Properly Sterilize and Store Instruments After Use”
},{
“@type”: “HowToStep”,
“text”: “Many infections caused by bacteria in hospital settings will respond to antibiotic treatment. Consequently, half of the patients in hospitals receive antibiotics. When prescribing antibiotics to treat HAIs, choose medicines to specifically target the pathogens causing the problem.”,
“name”: “Be Mindful When Prescribing for HAIs”
},{
“@type”: “HowToStep”,
“text”: “Handwashing is a key factor in preventing pathogen spread, but it’s often inadequate or overlooked by health care workers. Before blaming staff members for negligence, a surveyed group of health care workers reported 24 reasons for not practicing adequate hand hygiene. Some reasons cited included assuming that sterile gloves replaced the need for handwashing, not knowing the impact of handwashing on pathogen spread and lack of training.”,
“name”: “Practice Proper Handwashing”
},{
“@type”: “HowToStep”,
“text”: “The traditional white coat worn by doctors presents a prime carrier for bacteria between patients, especially the pockets and ends of the sleeves. During wound inspection, doctors should change out of their white coats and wear a plastic apron to reduce HAIs. Facilities shouldn’t require white coats in examination settings, especially when doctors must inspect wounds or near other sources of infection.”,
“name”: “Change Out of White Coats for Wound Inspection”
},{
“@type”: “HowToStep”,
“text”: “How health care workers insert and maintain intravenous catheters needs reviews in facilities. The skin should undergo thorough disinfection with 70% isopropyl alcohol and dry thoroughly before cannula insertion. While using bacteria-impermeable clear adhesive to hold the cannulas for IV lines in place is popular, it provides a place for bacteria to grow in the trapped sweat and skin cells. Instead, use polyurethane adhesives that allow for less moisture and bacteria accumulation under the tape. Lastly, labeling IV administration sets with the date and time to change them 72 hours after placement can reduce bacterial growth and HAIs.”,
“name”: “Improve Intravenous Catheter Care”
},{
“@type”: “HowToStep”,
“text”: “Disinfect surfaces in patient areas and clean linens frequently. Between patients, disinfect their rooms with a bleach-based agent. In rooms, wash all linens at least once daily if any touch the ground or they become dirty for any reason. In non-patient areas, such as lounge rooms and nurses’ stations, keep the area cleaned daily to prevent spreading diseases from break areas to patient areas.”,
“name”: “Clean and Disinfect Surfaces”
},{
“@type”: “HowToStep”,
“text”: “Patients with highly contagious infections should move into isolation rooms to prevent others from contracting the infections. Health care providers of these patients should use isolation-appropriate personal protective equipment (PPE) to reduce infection spread.”,
“name”: “Isolate Patients”
},{
“@type”: “HowToStep”,
“text”: “For patients with airborne infections, place them in an AIIR that includes negative air pressure compared to outside rooms, return air passed through a HEPA filtration system and ensure at least six air exchanges per hour. For newly constructed or remodeled AIIRs, the requirement for air exchanges is 12 per hour.”,
“name”: “Use HEPA Filtration to Prevent Airborne Infection Transmission”
}]
}
Hospital-acquired infections (HAIs) are preventable complications from surgery or other hospital stays. By creating and implementing infection-control measures, you can reduce HAIs in your facility in a cost-effective way, protect patients and save lives.
Take steps now to make the changes throughout your medical facility, from the operating room to patient rooms, to make headway toward reducing HAIs and improving care.
What Is a Hospital-Acquired Infection?
Hospital-acquired infections, also known as nosocomial infections, happen when patients get infections during treatment in a medical facility. These preventable issues happen too often, with one in 31 patients in hospitals having an HAI every day in the United States. Knowing the risk factors and types of HAIs you face in your facility will help you in establishing your facility’s plan for prevention.
Risk Factors for HAIs
Several factors increase the risk of hospital-acquired infections in patients:
- Long hospital stays
- Surgery
- Broken skin
- Invasive equipment used
One of the most important risks for HAIs is a long hospital stay. Typically, longer stays correlate to more complex conditions or multiple illnesses. The extended time in a medical facility and the higher likelihood of complicating illnesses increase the chances of nosocomial infections.
Surgery is another major factor in patients developing HAIs because it introduces another source of infection through surgical incisions. Additionally, longer surgeries put patients in the operating room and expose them to potential pathogens in that space for more time. During recovery, they may also have urinary catheters or IV lines that can become sources of infection.
Patients that have non-intact skin, such as cuts, burns or ulcers, have entry points for bacteria that may cause HAIs. Care for these open wounds requires exceptionally clean environments. Health care providers must thoroughly wash their hands and use proven techniques to prevent infection spread and wound contamination.
Common equipment used in medical facilities can harbor bacterial growth and cause infections. Urinary catheters, IVs and respiratory equipment can lead to infections due to their invasive nature and from leaving them intact for extended times during recovery.
Types of Hospital-Acquired Infections
HAIs come in several forms from a variety of sources. Understanding the dangers patients face is essential to developing a plan to combat them.
The top two causes of death from HAIs are pneumonia and infections in the bloodstream, with each accounting for more than 35,000 and 30,000 deaths, respectively, each year. Additional infections that rank among the top causes of death include UTIs and surgical site infections. Other sites, such as wound infections, account for the remaining deaths.
Why Is It Important to Reduce Hospital-Acquired Infections?
Reducing HAIs is vital in providing good medical care to patients. These infections are both deadly and costly. Each year, an estimated 99,000 patients die from HAIs. To cover additional care for these patients, hospitals spend between $96 and $147 billion each year. Knowing how to reduce the spread of infection in the OR and beyond can save lives and money.
How to Reduce Hospital Acquired Infections in the OR
The first step toward reducing HAIs in any health care facility starts with creating a plan for identifying and addressing the most common pathogens in your facility. You must make sure everyone knows the best practices for preventing infection spread and follows through with them every time they care for patients.
Consistent improvement in reducing infection spread takes time and effort, but the reduction in HAIs will reward the work. Here are a few steps to take to reduce the spread of infection in the OR at your facility:
1. Create an Antimicrobial Control Team
Establish an in-house team at your facility to combat HAIs. This team should identify the following:
- Sources of HAIs
- Barriers to preventing infection spread
- Ways to measure performance
- Spreading information to teams to ensure every patient gets equal HAI preventative care
On the team should be at least one expert in diseases and their spread. This professional can help team members identify means of pathogen transmission in ORs and other parts of the hospital and how to prevent them. The infectious diseases expert should also serve as a consultant for renovations or construction projects to ensure the facility has a protective design against disease spread.
This team will lead the movement toward making changes in operations and practices in reducing HAIs throughout your facility. Part of the job of the team will be to monitor and document information about the environment. This data will help with identifying areas for improvement.
Keep track of the following as recommended by the CDC:
- Create a plan for responding to water damage within 72 hours to prevent mold growth.
- Test samples of water used for medical services, such as in hemodialyzers, for bacteria.
- Look for potential environmental sources of bacterial growth and correct them.
- Keep track of positive airflow in protective environment spaces and negative airflow in patient isolation rooms.
By taking a team approach, other members of the staff will have support for making the changes needed to improve patient care and HAI reduction.
2. Identify Problem Pathogens
Identify the pathogens that have affected patients in your facility infected with HAIs. By knowing the specific diseases causing infections, physicians can avoid unnecessarily prescribing antibiotics.
Additionally, train staff on the pathogens that appear most often in your facility and other potential infection sources. Staff members should know what they’ll face and how the diseases spread. Some bacteria are airborne while others spread through surface contact or blood contamination.
Incoming patients with diarrhea or respiratory illnesses need testing to see if they have infections caused by bacteria that could spread through the facility. Isolating some of these patients, such as those with airborne diseases, may help reduce the spread of illnesses to others at the facility.
3. Properly Sterilize and Store Instruments After Use
Any instruments or equipment that come into direct contact with body fluids or sterile body tissues fall under the category of critical items. Properly done, sterilization kills all microorganisms on the surfaces of medical instruments. On the other hand, improperly sterilized equipment raises the risk of pathogen transmission.
During autoclaving, make sure to secure instruments in a container to keep them protected and allow for complete sterilization. Reusable sterilization containers that double as storage units provide a simple solution to ensuring the cleanliness of instruments used in the OR. The rigid exterior doesn’t break or rip, protecting the sterility of the instruments inside. These cases should become part of your instrument sterilization to reduce HAIs in the OR.
4. Be Mindful When Prescribing for HAIs
Many infections caused by bacteria in hospital settings will respond to antibiotic treatment. Consequently, half of the patients in hospitals receive antibiotics. When prescribing antibiotics to treat HAIs, choose medicines to specifically target the pathogens causing the problem.
Being deliberate in prescribing antibiotics can reduce resistant bacterial infections in your facility. Too much, unnecessary or inappropriate antibiotic use leads to resistant bacteria that don’t respond to traditional treatments. These pathogens include the following:
- VRE, also known as vancomycin-resistant Enterococcus
- MRSA, which is also called methicillin-resistant Staphylococcus aureus
- CRE, also referred to as Carbapenem-resistant Enterobacterales
- C. diff, Clostridioides difficile or C. difficile
- ESBL-producing Enterobacterales, or extended-spectrum beta-lactamase-producing Enterobacterales
Among these resistant bacteria, the top three are C. diff, which causes 12,800 annual deaths, MRSA, leading to 10,600 deaths and ESBL-producing Enterobacterales, resulting in 9,100 deaths. Addressing these resistant bacteria and others can save tens of thousands of lives each year.
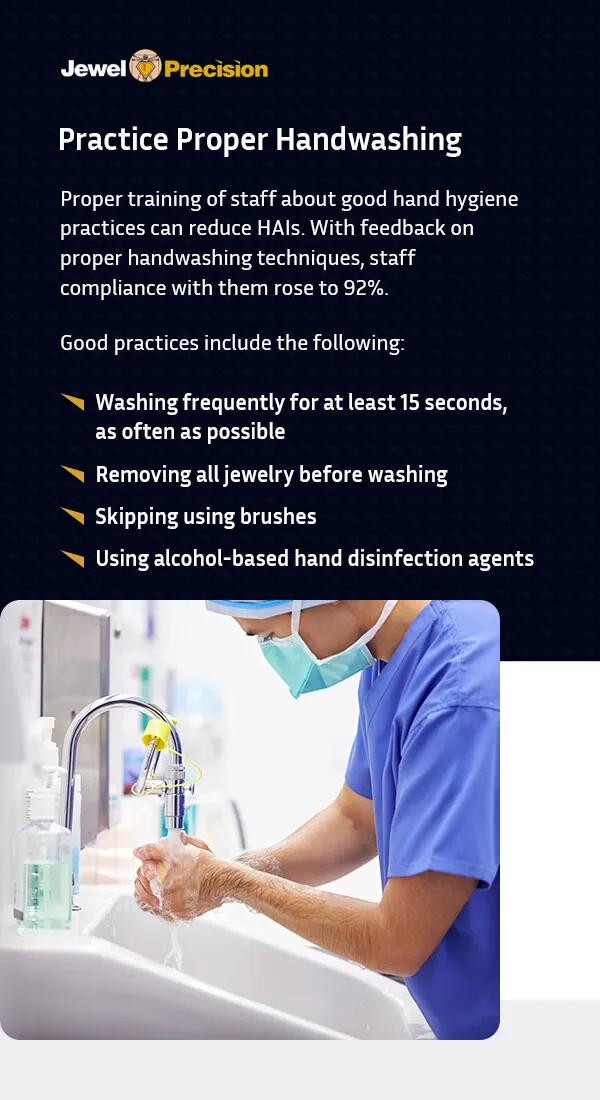
5. Practice Proper Handwashing
Handwashing is a key factor in preventing pathogen spread, but it’s often inadequate or overlooked by health care workers. Before blaming staff members for negligence, a surveyed group of health care workers reported 24 reasons for not practicing adequate hand hygiene. Some reasons cited included assuming that sterile gloves replaced the need for handwashing, not knowing the impact of handwashing on pathogen spread and lack of training.
Another reason staff may not practice good hand hygiene is in situations where they fill in during understaffed times or feel overworked. A study showed that good handwashing practices happened 25% of the time in understaffed facilities or by overworked staff members. When staff returned to their normal operations, good hand hygiene practice rates increased to 70%.
Proper training of staff about good hand hygiene practices can reduce HAIs. With feedback on proper handwashing techniques, staff compliance with them rose to 92%. Good practices include the following:
- Washing frequently for at least 15 seconds, as often as possible
- Removing all jewelry before washing
- Skipping using brushes
- Using alcohol-based hand disinfection agents
Even when wearing gloves, health care providers need to practice good handwashing techniques to prevent disease transmission and reduce HAIs.
6. Change Out of White Coats for Wound Inspection
The traditional white coat worn by doctors presents a prime carrier for bacteria between patients, especially the pockets and ends of the sleeves. During wound inspection, doctors should change out of their white coats and wear a plastic apron to reduce HAIs. Facilities shouldn’t require white coats in examination settings, especially when doctors must inspect wounds or near other sources of infection.
7. Improve Intravenous Catheter Care
IV lines are a prime source of bloodstream HAIs. Among those with critical illnesses, 25% of nosocomial infections stem from IVs, with a quarter of those cases resulting in death.
How health care workers insert and maintain intravenous catheters needs reviews in facilities. The skin should undergo thorough disinfection with 70% isopropyl alcohol and dry thoroughly before cannula insertion.
While using bacteria-impermeable clear adhesive to hold the cannulas for IV lines in place is popular, it provides a place for bacteria to grow in the trapped sweat and skin cells. Instead, use polyurethane adhesives that allow for less moisture and bacteria accumulation under the tape.
Lastly, labeling IV administration sets with the date and time to change them 72 hours after placement can reduce bacterial growth and HAIs.
8. Clean and Disinfect Surfaces
Disinfect surfaces in patient areas and clean linens frequently. Between patients, disinfect their rooms with a bleach-based agent. In rooms, wash all linens at least once daily if any touch the ground or they become dirty for any reason.
In non-patient areas, such as lounge rooms and nurses’ stations, keep the area cleaned daily to prevent spreading diseases from break areas to patient areas.
9. Isolate Patients
Patients with highly contagious infections should move into isolation rooms to prevent others from contracting the infections. Health care providers of these patients should use isolation-appropriate personal protective equipment (PPE) to reduce infection spread.
Those in these rooms should wear protective masks when moved outside their rooms to prevent spreading infection through droplets. Further, all patients should wear shoes when walking within or outside their rooms to avoid picking up germs from the floor or spreading germs outside their rooms.
10. Use HEPA Filtration to Prevent Airborne Infection Transmission
For patients with airborne infections, place them in an AIIR that includes negative air pressure compared to outside rooms, return air passed through a HEPA filtration system and ensure at least six air exchanges per hour. For newly constructed or remodeled AIIRs, the requirement for air exchanges is 12 per hour.
These measures keep potentially contaminated air within the patient’s room through negative air pressure. HEPA filtration can reduce HAIs by decreasing fungal spore and pathogen counts in rooms of immunocompromised patients.

Start Reducing Infections From the Operating Room With Jewel Precision Sterilization Cases
Reducing infections requires a multifaceted approach to pathogen control. Proper sterilization and storage of instruments is one part of that. With Jewel Precision reusable sterilization cases, you can organize and protect instruments through autoclaving while reducing waste and cost.
These durable, rigid cases can withstand more than 100 cleaning processes without showing evidence of hemoglobin or proteins on them. Replaceable filters on the cases cut waste and cost compared to easily torn, wasteful blue wrap. We also have custom and modular sterilization cases to choose from.
Start using these cases for your OR instruments to prevent infection spread by contacting us at Jewel Precision.