
Robotic surgery helps surgeons perform some of the most intricate procedures in modern hospitals and medical facilities. These operations wouldn’t be possible without the help of specialized instruments. Ensuring that the instruments used in robotic surgery are adequately sterilized and pathogen-free is crucial for patient safety.
Learn some best practices and techniques for cleaning and sterilizing your robotic surgical instruments so you can protect your patients and prolong the instruments’ life span.
What Are Robotic Surgery Instruments?
Robotic surgical instruments are advanced tools designed to assist surgeons during robotic surgery or robotic-assisted surgery (RAS). RAS procedures are typically minimally invasive and designed to minimize complications while increasing surgeon precision. This is made possible through the delicate, complex tools that allow for smaller incisions while giving the surgeon better vision.
These surgical tools are part of a larger robotic system, where the surgeon (aided by cameras and high-definition imaging) controls the instruments through a console during the surgery.
What Are Robotic Surgery Instruments Used For?
The first introduction of RAS into medicine was back in 1980 by the Robotics Institute at Carnegie Mellon University. It developed a programmable “assistant” to perform various tasks such as moving materials, parts and tools from one point to another.
A few years later, in 1988, the first RAS was performed. It was a brain biopsy, and the surgical team used the Programmable Universal Manipulation Arm (PUMA) 560 robot to guide a needle (under CT guidance) into the patient’s brain. This was possible because of the PUMA’s six degree-of-freedom flexible arm.
There have been many advancements since then. More recently, the military (approved by the FDA) helped fund the development of the da Vinci Surgical System in 2000. This system uses robotic tools to facilitate complex intracavitary surgeries. Currently, several systems use robotics for spinal procedures, particularly because they help with precision.
RAS instruments continue to grow and are used in a variety of medical procedures. They are particularly useful in complex procedures where certain areas may be challenging to reach. These include operations in the following disciplines:
- Cardiology: Robotic tools can help a surgeon make the necessary incisions and perform more delicate work in the chest cavity for procedures like coronary artery bypass grafting (CABG).
- Urology: A prostatectomy (the removal of the prostate) is a delicate procedure. Instruments of robotic surgery make navigating through sensitive areas more achievable.
- Orthopedic procedures: When surgeons need to perform replacement procedures (for example, hip replacement surgery), robotic instruments can assist them in accurately aligning and replacing the artificial joints.
- Gynecology: Robotic surgical tools allow for more accurate and delicate work in popular gynecology procedures such as hysterectomies or myomectomies.
Different Types of Robotic Surgical Instruments
Surgeons typically use mechanical arms and a camera arm for robotic surgery. The arms have a great range of motion (more than the human wrist), and each has a different instrument attached to perform tasks such as clamping, dissecting or suturing. Some of the most common robotic surgical instruments include:
- Robotic graspers
- Robotic clip applicators
- Robotic scissors
- Robotic needle holder and drivers
In addition, the camera arm has image processing equipment and a high-definition 3D endoscope.
What Surgical System Uses Robotic Instruments?
The medical field uses RAS systems to complete robotic surgery. The most common RAS system is the da Vinci Surgical System, which is currently used in 71 countries and has performed more than 14 million procedures worldwide.
This system has three main components:
- The surgeon console: This is where the surgeon sits and controls the instruments while getting a high-definition 3D view of the surgical site.
- The patient cart: Set alongside the patient’s bed, the patient cart holds the camera and additional instruments the surgeon controls from the console. These tools are necessary to move the arms and instruments that work inside the patient. Each instrument has a piece that connects with the robotic arm, a shaft that houses the cables that help operate the wrist, and a tip that may be a needle driver, grasper, scissors, cautery tip or any other function.
- The vision cart: This allows seamless communication between components and supports a 3D high-definition vision system.
How to Clean Robotic Surgery Instruments
The cleaning and sterilizing of robotic surgical instruments should follow standard CDC procedures to avoid possible cross-contamination between patients and the buildup of biofilms. Reprocessing robotic surgical instruments can also increase the instruments’ life span and decrease the turnaround time between procedures.
Manual Cleaning of Robotic Instruments
Manually cleaning robotic surgery accessories starts with the pre-cleaning phase. Pre-cleaning helps ensure that later cleaning of the tools is more effective. Many robotic surgical tools are designed with detachable parts. After surgical use, the tools are disassembled and treated with a gel. The gel helps loosen and prevent the drying of any soil (for example, blood, bone and tissue) on the instruments.
For manual cleaning, the surgical tools will then be transported to a dedicated decontamination area of the Sterile Processing Department (SPD). Upon arrival, the instruments will be removed from the container and assembled. During this stage, the staff will ensure that all surfaces are exposed while they manually clean the instruments using a three-bay sink. Each bay has a different purpose:
- Bay one: The staff will pre-rinse the tools with cold water to remove the gel used from the previous step. At this point, any blood, bone or tissue will also be gently removed.
- Bay two: After the cold water rinse, the staff will then place the instruments in a neutral or enzymatic solution (this depends on the type of instrument). The enzymatic cleaner typically has a pH of 6-8 and helps break down soils.
- Bay three: The third bay is for rinsing the instruments. The specific treatment used here will depend on the manufacturer’s recommendation. For example, high-pressure water may cause spotting, while chloride levels can damage some tools. Following the manufacturer’s recommendations here is crucial.
Automated Cleaning of Robotic Instruments
Automated cleaning is an invaluable step. It involves ultrasonic cleaning and washer-disinfector cleaning to ensure instruments are thoroughly sanitized and ready to be placed in an autoclave:
- Ultrasonic cleaning: Some robotic surgical instruments have crevices and hinges that are challenging to reach and clean manually. Ultrasonic cleaning machines can help. First, separate the tools based on their metals. Once they are placed inside the ultrasonic cleaner, the machine will create high-frequency ultrasonic waves to help dislodge any soil from the instruments’ surface. Ensure that each item gets direct exposure to the waves. You can run the cycle according to the manufacturer’s guidelines (typically around 10-15 minutes). After this process, all the tools must be rinsed with softened or deionized water.
- Washer-disinfector cleaning: After ultrasonic cleaning, the instruments are placed in a washer-disinfector, where pressurized water is sprayed at a specific water temperature, flow rate and chemical concentration. You’ll need to place the tools so that the water and disinfector contact all the surfaces. Some washer-disinfectors have drying cycles that are suitable for these delicate robotic instruments. While drying, it’s essential to ensure that the temperature meets the manufacturer’s guidelines.
Can Robotic Instruments Go in an Autoclave?
When selecting your sterilization method, consider what is best for your facility’s materials. Steam sterilization in an autoclave is a popular choice among hospitals and other medical facilities for reprocessing robotic accessories. With this route, you will likely benefit from a greater chamber and larger load capacity that autoclave systems typically offer.
Autoclave systems help hospitals and medical facilities with sterilizing robotic instruments and materials. They use pressurized steam at a set temperature and pressure for a particular period.
While autoclave systems are crucial in sterilizing many surgical tools, only certain instruments can safely go inside an autoclave, including:
- Forceps
- Scissors
- Implants
- Syringes
- Scalpels
- Hemostats
- Screws
- Plates
- Implantable medical devices
In addition, you can sterilize the following medical materials in an autoclave:
- Glassware
- Centrifuge tubes
- Chemical solutions
- Hospital linens
- Autoclavable plasticware
- Pipette tips
- Biomedical waste
Understanding which materials you can safely place in an autoclave is essential for your staff’s safety. Placing the wrong materials might lead to:
- An explosion: If the autoclave door malfunctions, the heat and pressure that will escape from the chamber can result in an explosion.
- Burning: Placing the incorrect instrument in your autoclave system can lead to fires. The machine reaches high temperatures, which can result in severe burns for those loading or unloading the autoclave.
- Melting or shattering: If the instruments you place inside the autoclave cannot withstand high temperatures, they may eventually melt or shatter.
- Machine damage: When you place an item into the autoclave that isn’t suitable for the system, you risk damaging the machine.
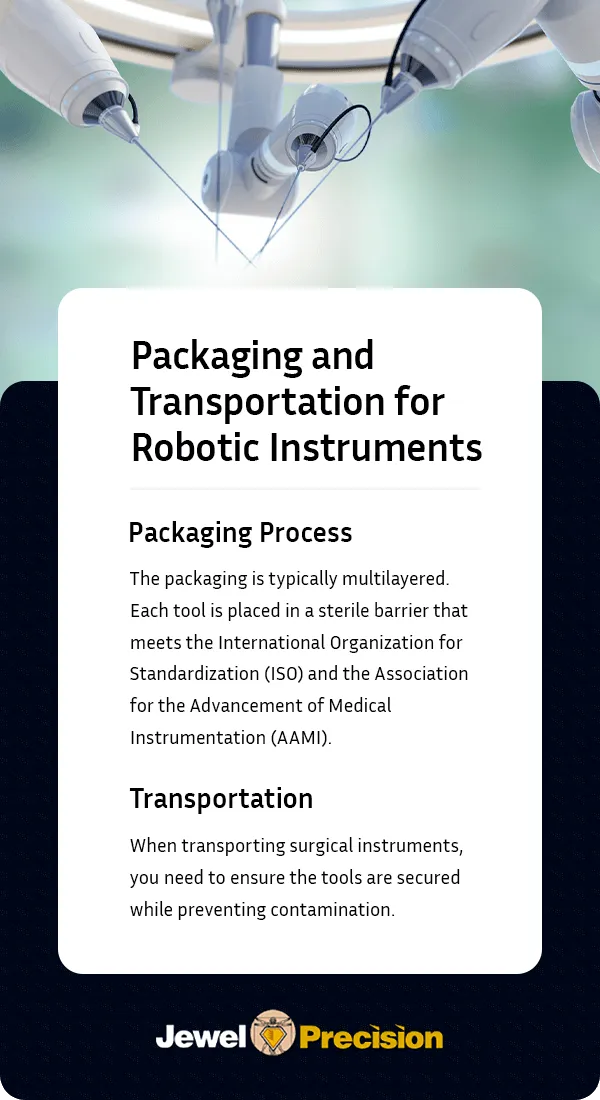
Packaging and Transportation for Robotic Instruments
The packaging and transporting of robotic surgical instruments is essential in safeguarding these tools against contamination, damage or functional impairment. Since the instruments play an integral role in the surgical outcomes and are often costly to repair or replace, this process requires thorough planning.
Packaging Process
Surgical instrument packaging must be carefully designed to protect the tools from environmental contaminants, moisture and physical impacts that may occur while they are being transported.
The packaging is typically multilayered. Each tool is placed in a sterile barrier that meets the International Organization for Standardization (ISO) and the Association for the Advancement of Medical Instrumentation (AAMI).
This container needs to keep out dust and microorganisms. It should also protect your sterile robotic instruments until they’re ready for use. Instruments with sharp edges or protruding parts (for example, scissors or scalpels) need to be cushioned within the pouch to prevent punctures.
Transportation
When transporting surgical instruments, you need to ensure the tools are secured while preventing contamination. For example, excessive heat or cold moisture may compromise the instruments’ sterilization status.
During transportation, the robotic surgical tools should be in a container that has:
- Shock protection: Packaging solutions that are designed with shock absorption and padding can help minimize some of the impact that may come from traveling.
- Humidity and temperature control: The ideal temperature recommendation from the manufacturer’s guidelines must be maintained.
Robotic instruments can be challenging to work with. For example, most come with a maximum number of uses. Using specialized trays to individually pouch your tools can help. This way, you’ll only clean and sterilize the individual tools you’ve used, helping ensure you don’t “waste” the instruments.
Procuring dependable surgical instrument organization systems designed for durability and efficiency is the key to shielding your medical tools from harsh environments.
Jewel Precision designs custom container systems that protect your valuable instruments and materials while in an autoclave. We’re the first to design medical sterilization trays, making us pioneers in our field. Our process for delivering custom cases to your medical facilities includes three steps:
- Discovery: In our initial consultation, our team will discuss your needs regarding surgical instrument cases and trays. How big or small do you need the trays to be? What types of instruments will they carry? How many cycles will they typically go through the autoclave? Understanding your unique needs will help us create the most suitable containers for you.
- Design: At this stage, we’ll begin designing your surgical sterilization tray or case. We’ll draft each item with careful attention to detail and ensure that it meets your needs.
- Manufacturing: After finalizing your custom design, we’ll manufacture your cases and trays.
- Delivery: We’ll deliver your custom cases and trays to your medical facility so you can begin using them.

Sterilize Your Robotic Surgical Instruments With Jewel Precision
Every surgeon needs sterile equipment that’s safe to use on their patients. Jewel Precision develops high-quality autoclave sterilization cases and trays that keep your instruments sterile, organized and secure. We construct these cases with the best materials to help them withstand extreme sterilization conditions while protecting your tools. We can also help you customize your cases based on your needs. Contact us today to learn more about our products and services.